Why Bone Loss Happens After Tooth Extraction
When you lose a tooth, your jawbone changes. The bone that once supported your tooth starts to shrink and weaken because it no longer gets pressure and stimulation from chewing.
This process starts quickly and can change your jaw structure over time.

Many patients do not realize what happens beneath their gums. Bone loss can affect your facial appearance, make future dental implants harder, and impact the stability of your remaining teeth.
Understanding this process helps you protect your oral health.
You can take steps to keep your jawbone healthy after tooth loss. Dentists offer several methods to preserve your bone and prevent further problems.
Learning about these options now can help you avoid complicated and costly treatments later.
Key Takeaways
- Your jawbone starts to shrink after tooth extraction because it loses chewing stimulation.
- Bone loss can change your facial shape and make dental treatments harder.
- You can prevent bone loss with procedures like bone grafting and dental implants.
Why Bone Loss Happens After Tooth Extraction

When you lose a tooth, your jawbone begins to shrink because it stops receiving the stimulation needed to stay strong. Your body recognizes the bone is no longer needed and starts to break it down through bone resorption.
The Role of Tooth Roots in Jawbone Health
Tooth roots do more than hold your teeth in place. Every time you chew or bite, the roots send pressure to the surrounding jawbone.
This pressure signals your body to keep the bone strong. The jawbone rebuilds itself in response to this stimulation.
When a tooth is removed, the root goes with it. The bone stops getting signals that it is needed.
Your body shifts nutrients away from the unused area. Within weeks of tooth extraction, bone resorption begins as minerals move to other parts of your body.
Understanding Bone Resorption
Bone resorption is your body’s process of breaking down bone tissue and absorbing the minerals. Special cells called osteoclasts dissolve the bone and release calcium and other minerals into your bloodstream.
This process happens throughout your body but speeds up after you lose a tooth.
Normally, bone breaks down and rebuilds in balance. After tooth loss, breakdown happens faster than rebuilding because there is no stimulation.
The bone in the extraction site becomes thinner and weaker.
Timeline and Progression of Bone Loss
The most bone loss happens in the first year after extraction. Studies show you can lose up to 25% of bone width in that time.
Bone height also decreases, but usually more slowly.
Here’s what usually happens:
- First 3 months: Rapid bone loss starts right away, with the biggest changes in this period.
- Months 3-12: Bone loss continues but slows down.
- After year 1: Bone continues to shrink, losing about 0.5% of density each year.
The rate of bone loss depends on your age, oral health, and overall bone density.
Risk Factors That Accelerate Bone Deterioration
Some factors can make bone loss happen faster after tooth extraction. Gum disease is a major risk because it damages both gums and bone even before tooth removal.
If you had gum disease, you may have lost bone before the extraction.
Poor oral hygiene allows bacteria to harm the extraction site and nearby bone. Age is also a factor, since bone density decreases as you get older.
Other risk factors include:
- Smoking or tobacco use
- Certain medications like corticosteroids
- Medical conditions such as osteoporosis or diabetes
- Hormonal changes, especially in postmenopausal women
- Using dentures for a long time without proper support
If you are missing several teeth, you lose more bone because larger areas are unused. The longer you wait to replace missing teeth, the more bone you lose.
Consequences of Bone Loss After Tooth Removal
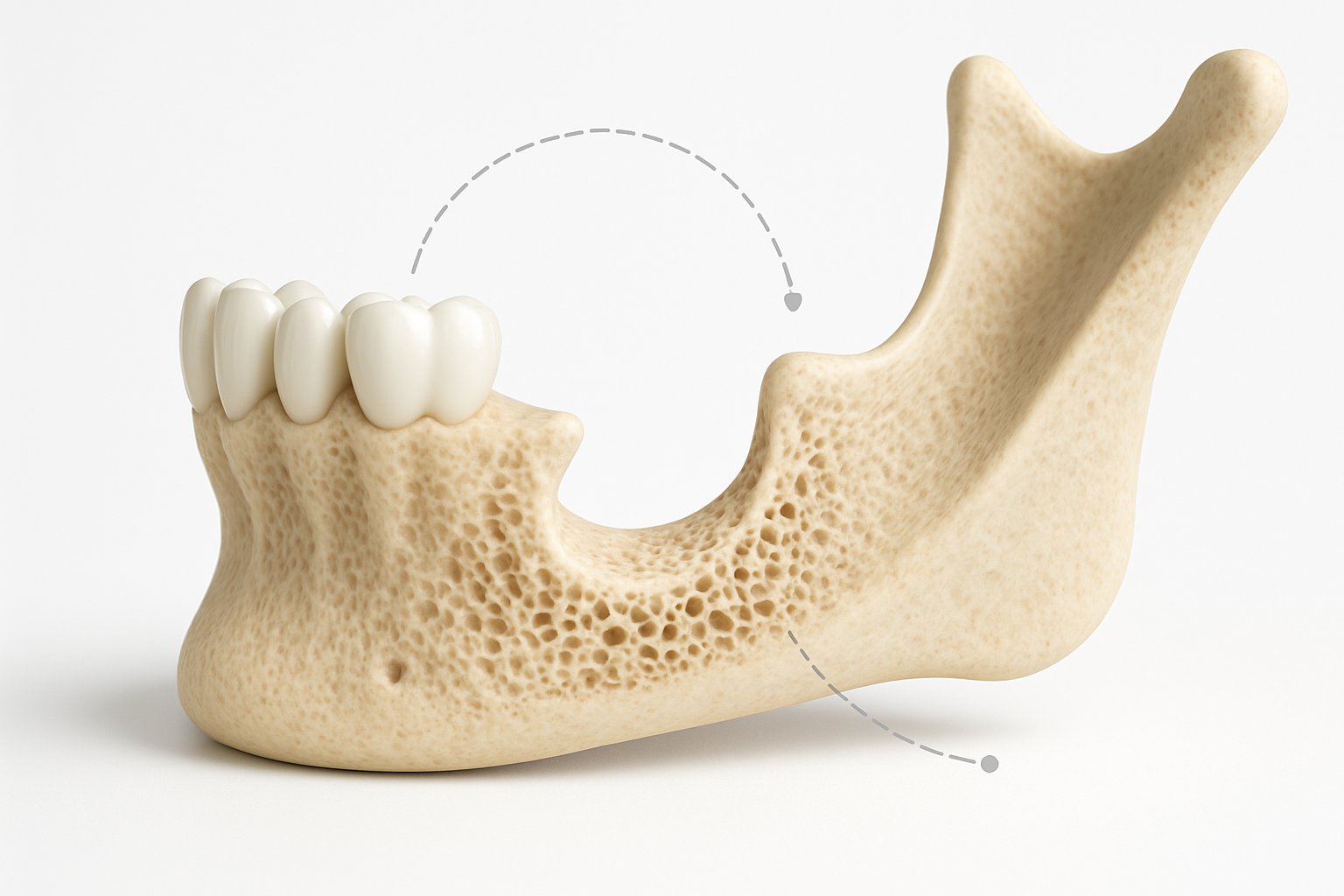
When bone loss happens after tooth extraction, it can cause problems beyond the empty space. The jawbone shrinks over time, which affects your facial shape, nearby teeth, and your options for tooth replacement.
Impact on Facial Structure and Appearance
Bone loss in your jaw changes your face. The jawbone supports your facial muscles and skin, much like a tent frame holds up fabric.
When you lose bone, your face can start to look sunken, especially near the mouth and cheeks. Your lips may look thinner and fold inward.
The lower part of your face can appear shorter. These changes can make you look older.
The chin may become more pointed as the jawbone shrinks. Deep wrinkles and lines around the mouth may become more obvious.
Effects on Tooth Alignment and Shifting Teeth
Teeth next to an extraction site move when bone disappears. They drift into the empty space, causing alignment problems.
Common shifting patterns include:
- Neighboring teeth tilt toward the gap.
- Opposite teeth grow into the space.
- Front teeth become crooked or crowded.
- Your bite changes.
This movement happens slowly over time. You may not notice it at first, but eventually, your teeth do not fit together as they should.
Shifting teeth can create new gaps and make chewing harder.
Challenges for Tooth Replacement and Dental Restorations
Bone loss makes it harder to replace missing teeth. Dental implants need enough bone to anchor in the jaw.
If you lose too much bone, you may need bone grafting before getting an implant.
Bridges are harder to fit when the bone shrinks. Gaps can form under the bridge, trapping food and causing discomfort.
Dentures are most affected by bone loss. As your jawbone shrinks, dentures become loose and unstable.
You may need frequent adjustments or replacements. Many people struggle with slipping or sore dentures due to poor bone support.
Long-Term Oral Health Complications
Ongoing bone loss weakens the jaw and affects your remaining teeth. The remaining teeth take on more chewing pressure, which can wear them down or cause breakage.
You risk losing more teeth as bone support weakens. Your bite force drops, making it harder to eat healthy foods.
Jaw pain and TMJ problems can develop as your bite changes. You may have headaches or trouble opening your mouth fully.
Lower bone density can make future dental procedures harder.
How to Prevent Bone Loss After Tooth Extraction

You can take steps to protect your jawbone after losing a tooth. The most effective ways include surgical techniques during extraction, replacing missing teeth with implants, good oral care, and a healthy diet and lifestyle.
Socket Preservation and Bone Grafting Techniques
Dentists can perform socket preservation right after tooth extraction to keep the shape and density of your jawbone. They fill the empty socket with bone graft material before the gum heals over it.
The bone graft acts as a scaffold for new bone to grow. Dentists use different types of grafts, including natural bone, synthetic materials, or animal-derived products.
Common bone grafting materials include:
- Autografts (from your own body)
- Allografts (from human donors)
- Xenografts (from animal sources)
- Alloplasts (synthetic materials)
Bone grafts help keep up to 90% of the original bone volume. This makes future dental implants easier and more successful.
Dental Implants for Jawbone Stimulation
Dental implants are the only tooth replacement that stops ongoing bone loss. The implant post acts like a natural tooth root, sending chewing pressure into the jawbone.
This stimulation keeps bone cells active and strong. Dentists usually recommend placing implants as soon as the site heals, often within three to six months.
Early implant placement prevents rapid bone loss in the first year. Sometimes, dentists can place an implant on the same day as extraction.
The titanium post fuses with the bone—a process called osseointegration. This creates a stable base and preserves bone for many years.
Without this stimulation, the jawbone can lose 25% of its width in the first year.
Immediate Post-Extraction Care and Oral Hygiene
Proper care after extraction helps protect the blood clot that forms in the socket. This clot is important for bone healing.
Avoid disturbing it by not smoking, using straws, or rinsing too hard.
Keep the area clean by gently rinsing with warm salt water after 24 hours. Brush your teeth carefully, but avoid the socket for the first few days.
Follow all post-op instructions, including taking any prescribed medicine. If you have heavy bleeding, severe pain, or signs of infection, contact your dentist right away.
Good oral hygiene during healing helps healthy bone form and prevents problems.
Lifestyle and Dietary Strategies for Bone Health
Your bones need certain nutrients to stay strong after tooth extraction. Calcium is the main building block of bone.
Adults need 1,000 to 1,200 milligrams of calcium daily from foods like dairy, leafy greens, and fortified products.
Vitamin D helps your body absorb calcium. You get vitamin D from sunlight, fatty fish, egg yolks, and fortified foods.
Most adults need 600 to 800 IU of vitamin D each day.
Key nutrients for bone health:
| Nutrient | Daily Amount | Food Sources |
|---|---|---|
| Calcium | 1,000-1,200 mg | Milk, cheese, yogurt, kale, broccoli |
| Vitamin D | 600-800 IU | Salmon, tuna, egg yolks, fortified milk |
| Protein | 0.8 g per kg body weight | Meat, fish, beans, nuts |
| Vitamin K | 90-120 mcg | Leafy greens, Brussels sprouts |
Avoid smoking and limit alcohol because both slow bone healing. Regular weight-bearing exercise helps keep bones strong, including your jawbone.
Stay hydrated and eat a balanced diet to support healing.
Restoring Bone Loss and Advanced Treatment Options
When bone loss has already happened, dentists offer several treatments to rebuild and restore your jawbone. These options range from basic bone grafts to advanced solutions for replacing multiple missing teeth.K
Bone Regeneration Procedures
Bone grafting is the most common method we use to restore lost jawbone tissue. During this procedure, we place grafting material into the area where bone has deteriorated.
The graft can come from your own body, a donor, an animal source, or synthetic materials. The grafting material acts as a scaffold.
New bone cells grow into and around the graft over several months. We call this process osseointegration.
We usually wait 3 to 6 months after bone grafting before placing dental implants. This waiting period allows the new bone to become strong and dense enough to support the implant.
Guided bone regeneration (GBR) is a technique we often combine with bone grafting. We place a special membrane over the graft material to protect it and direct bone growth.
The membrane keeps soft tissue from growing into the area while bone develops underneath. This helps ensure successful bone regeneration.
All-on-4 and Full-Arch Dental Implant Solutions
The All-on-4 system uses just four dental implants to support a full arch of replacement teeth. We angle the back implants at 45 degrees to avoid areas with significant bone loss.
This design often eliminates the need for bone grafting. Patients with moderate to severe bone loss benefit from this approach.
We anchor the angled implants into stronger bone areas that typically resist deterioration. Often, we can attach temporary teeth on the same day as implant placement.
Full-arch solutions like All-on-4 restore function and appearance while preventing further bone loss. The implants stimulate the jawbone like natural tooth roots.
Sinus Lift and Ridge Augmentation
A sinus lift becomes necessary when bone loss occurs in the upper back jaw near the sinuses. We gently lift the sinus membrane and place bone graft material underneath it.K
This creates enough bone height to place dental implants in the upper jaw. There are two types of sinus lifts:
- Lateral window approach: We use this when significant bone building is needed.
- Crestal approach: We use this for minor bone addition.K
Ridge augmentation rebuilds the width and height of the jawbone ridge. When teeth are missing for a long time, the ridge becomes narrow and weak.
We add bone graft material along the ridge to expand it. This creates a stable foundation for dental implants or other restorations.
Monitoring and Maintaining Jawbone Health
After any bone restoration procedure, we monitor healing through regular dental visits and X-rays. Digital imaging helps us see how well new bone is developing.
We usually take X-rays at 3 months, 6 months, and 12 months after treatment. Good oral hygiene protects your investment in bone regeneration.
Brush twice daily and floss around any implants or dental work. Avoid smoking, as it slows bone healing and increases treatment failure rates.
We recommend calcium and vitamin D supplements to support bone health. A balanced diet with adequate protein also helps bone regeneration.
Contact us immediately if you notice pain, swelling, or loosening of dental work.
Frequently Asked Questions
Bone loss after tooth extraction usually begins within the first few months. The rate depends on the location and individual factors.
Several dental procedures can preserve or rebuild bone, including grafts and implants placed soon after extraction.
What methods are effective in preventing bone loss after a tooth is removed?
We recommend socket preservation as the most effective method to prevent bone loss. This involves placing bone graft material into the empty socket immediately after extraction.
The graft acts as a scaffold for new bone to grow. Dental implants also prevent bone loss by mimicking natural tooth roots.
When we place an implant, it stimulates the surrounding bone through normal chewing forces. This keeps the bone active and healthy.
Another option is ridge preservation, which uses a membrane to cover the graft material. We often combine this with platelet-rich fibrin to speed up recovery.
Can bone growth be stimulated post tooth extraction, and if so, how?
Yes, we can stimulate bone growth after extraction through bone grafting procedures. We use materials like autografts (from your own body), allografts (from donors), or synthetic options.
These materials encourage your body to create new bone cells. Growth factors and proteins can enhance bone formation.
We sometimes apply these substances directly to the extraction site. They signal your body to send more healing cells to the area.
Dental implants themselves stimulate ongoing bone growth. The titanium post fuses with your jawbone through a process called osseointegration.
This creates pressure that tells your body to maintain bone density in that spot.
At what rate does bone loss typically occur following the removal of a tooth?
The first three to six months show the most significant bone loss. We observe that about 40-60% of bone width can disappear during this period.
The height of the bone ridge typically decreases by several millimeters. Front teeth areas lose bone faster than back teeth areas.
This happens because the bone around front teeth is naturally thinner. The outer wall of bone is especially vulnerable to shrinkage.
After the initial six months, bone loss continues but at a slower pace. The total bone loss over time depends on factors like age, genetics, and oral health habits.
Is bone regeneration possible after the extraction of a tooth, and what are the best practices?
Bone regeneration is possible even years after extraction. We perform bone grafting procedures to rebuild lost bone structure.
The success rate depends on how much bone you’ve lost and your overall health. The best practice is to act quickly after extraction.
We prefer to place grafts during or immediately after tooth removal. This prevents bone loss rather than trying to fix it later.
We assess your bone density with 3D imaging before planning regeneration. Good oral hygiene and not smoking improve your chances of successful bone growth.
Adequate vitamin D and calcium intake also support bone healing.
Does the removal of wisdom teeth often result in bone loss?
Wisdom tooth removal can cause bone loss in the back of the jaw. However, the impact is usually less noticeable than losing front or middle teeth.
The bone in wisdom tooth areas tends to fill in better naturally. Most people don’t need bone grafts after wisdom tooth extraction.
We only recommend grafts if you plan to place implants in those areas later. Young patients typically experience better natural bone healing than older adults.
What is the typical timeframe for bone loss to begin after a tooth has been extracted?
Bone loss starts immediately after a tooth is removed. The most rapid changes happen within the first two weeks.
You can lose noticeable bone width within the first month. By three months, most bone remodeling has finished.
At this stage, softer and less dense bone fills the socket. The bone keeps hardening and changing shape for up to a year.
Without treatment, bone loss continues at a slow pace over time.
📞 Contact Kaufman Dentistry Today
Give us a call at (310) 838-7780 to schedule your appointment and take the first step towards a stunning smile.
You can find us at 10760 Washington Blvd., Culver City, CA 90232. We look forward to welcoming you to our practice and helping you achieve the smile of your dreams!
