Diabetes and Oral Health

Diabetes affects millions of people worldwide and creates serious challenges for oral health.
High blood sugar levels damage blood vessels and make it harder for the body to fight infections.
This situation makes the mouth more likely to develop gum disease and tooth decay.
People with diabetes experience a two-way relationship between their condition and oral health.
Diabetes makes oral problems worse, and gum disease makes blood sugar harder to control.
When glucose levels stay high, harmful bacteria multiply in the mouth.
Saliva may also have more sugar, which feeds the bacteria that cause cavities.
Good oral hygiene becomes even more important for people with diabetes.
With the right knowledge and daily habits, we can protect our teeth and support our overall health.
Key Takeaways
- Diabetes and gum disease affect each other and impact blood sugar control and oral health.
- High blood sugar raises the risk of tooth decay, gum disease, and other mouth infections.
- Daily brushing, flossing, and regular dental visits help people with diabetes maintain good oral health.
The Link Between Diabetes and Oral Health

High blood glucose levels damage oral tissues and weaken the immune system.
This cycle makes gum disease worse and raises blood sugar levels.
Impact of Blood Sugar on Oral Tissues
When blood glucose stays high, sugar builds up in saliva.
This extra sugar feeds harmful bacteria in the mouth.
The bacteria multiply quickly and form sticky plaque on teeth.
High blood sugar also lowers saliva flow, which usually helps clean the mouth.
Blood sugar weakens blood vessels in the gums and slows healing after dental work.
Tissues become more prone to infection and heal slowly.
Poor glycemic control thickens blood vessel walls, making it harder for nutrients and infection-fighting cells to reach gums and teeth.
The mouth becomes a good place for bacteria to grow when blood glucose stays high.
Even small cuts or irritation take longer to heal.
People with prediabetes or type 2 diabetes may notice their gums bleed more easily.
High blood sugar damages the tiny blood vessels that supply the gums.
Role of Inflammation and Immune Response
Diabetes causes chronic inflammation in the body, including the mouth.
High blood glucose triggers inflammation that harms healthy tissue.
The immune system works harder to control blood sugar.
This leaves fewer resources to fight oral infections and heal gums.
Inflammation makes gums red, swollen, and tender.
It also reduces the body’s ability to fight bacteria and slows tissue repair.
Insulin resistance makes inflammation worse.
When cells do not respond well to insulin, the body produces more inflammatory chemicals.
These chemicals attack both bacteria and healthy tissue.
Gums can suffer damage even with good oral hygiene.
Poor diabetes management increases the risk of severe oral problems.
The immune system struggles to control blood sugar and oral infections at the same time.
Bidirectional Relationship With Gum Disease
Periodontal disease and diabetes create a cycle that harms health.
Gum infections make blood sugar harder to control.
High blood glucose makes gum disease worse.
Active gum disease lets bacteria enter the bloodstream through inflamed gums.
The body releases stress hormones and inflammation to fight these bacteria.
Diabetes increases the risk of severe gum disease.
Gum disease makes blood sugar control more difficult.
Both conditions involve similar inflammatory pathways.
Treating one condition can help improve the other.
People with gum disease often need more insulin to manage blood glucose.
Inflammation from infected gums lowers insulin sensitivity.
Treating gum disease often leads to better blood sugar control.
Reducing gum inflammation helps the body use insulin more effectively.
Dentists may recommend diabetes screening for patients with severe gum disease.
Common Oral Health Problems in People With Diabetes

People with diabetes have higher risks for several mouth problems.
These include gum disease, dry mouth, infections, and tooth decay.
Gum Disease: Gingivitis and Periodontitis
Gum disease affects people with diabetes more often and more severely.
High blood sugar makes it harder to fight bacteria in the mouth.
Gingivitis is a mild form of gum disease.
Gums become red, swollen, and bleed easily.
Periodontitis is a severe form that develops when gingivitis goes untreated.
This condition destroys the tissue and bone that hold teeth in place.
Signs of periodontitis include receding gums, deep pockets between teeth and gums, persistent bad breath, loose teeth, and tooth loss.
Plaque builds up faster in people with diabetes.
The bacteria in plaque produce toxins that irritate gums.
Poor blood sugar control makes infections worse and harder to heal.
Dry Mouth and Saliva Reduction
Dry mouth, or xerostomia, is common in people with diabetes.
This happens when the salivary glands do not make enough saliva.
Saliva protects the mouth by washing away food and bacteria.
It also neutralizes acids that cause tooth decay.
Without enough saliva, harmful bacteria grow more easily.
High blood sugar, diabetes medications, and dehydration can cause dry mouth.
Dry mouth increases the risk of tooth decay, gum disease, difficulty swallowing, burning mouth, and bad breath.
We need saliva to keep our mouth healthy.
When saliva production drops, oral health problems get worse quickly.
Fungal and Bacterial Infections
People with diabetes get mouth infections more often.
High blood sugar creates an environment where harmful organisms grow easily.
Thrush is a common fungal infection.
It causes white patches on the tongue, cheeks, and roof of the mouth.
These patches can hurt and may bleed when scraped.
Bacterial infections can cause abscesses in the gums or around tooth roots.
These painful swellings fill with pus and need quick treatment.
Poor blood sugar control, dry mouth, weak immune system, and poor oral hygiene raise infection risks.
Fungal infections often return if blood sugar stays high.
We must control diabetes well to prevent these mouth problems.
Tooth Decay and Cavities
Tooth decay happens more often in people with diabetes.
High blood sugar in saliva feeds the bacteria that cause cavities.
The bacteria make acids that damage tooth enamel.
This creates holes called cavities.
Without treatment, decay spreads deeper into the tooth.
High blood sugar, low saliva flow, frequent snacking, and poor oral hygiene increase the risk.
Cavities can lead to abscesses and more serious infections.
Tooth decay can progress quickly in people with poorly controlled diabetes.
Regular dental checkups help catch cavities early.
Prevention and Self-Care Strategies

Good oral care and diabetes management protect your mouth and overall health.
Daily hygiene, blood sugar control, and healthy choices make a difference.
Daily Oral Hygiene Routines
Brush twice daily with fluoride toothpaste to remove plaque and bacteria.
Brush for two minutes using a soft-bristled toothbrush.
Replace toothbrushes every three months.
Floss daily to clean between teeth where brushes cannot reach.
Floss gently to avoid injuring gums.
Water flossers can help people with sensitive gums.
Use mouth rinse to kill bacteria and freshen breath.
Choose an antibacterial mouthwash after brushing and flossing.
Pick products without alcohol if you have dry mouth.
Daily Schedule:
- Morning: brush, floss, mouth rinse
- Evening: brush, floss, mouth rinse
- After meals: rinse with water
Clean your tongue every day with a tongue scraper or toothbrush.
This removes bacteria that cause bad breath and infections.
Role of Diabetes Management in Oral Health
Glycemic control directly affects oral health.
High blood sugar feeds harmful bacteria in the mouth.
Keep blood sugar in the target range set by your doctor.
Test blood sugar regularly to track your levels.
Check before meals and at bedtime.
Keep records to share with your healthcare team.
Take medications as prescribed.
Never skip insulin or diabetes medicines.
Missing doses leads to high blood sugar and gum problems.
Tell your dentist about your diabetes and medications.
Share dental problems with your diabetes doctor too.
Nutrition, Lifestyle, and Smoking Cessation
Eat a balanced diet to control blood sugar and support gum health.
Limit sugary foods and drinks that feed mouth bacteria.
Choose whole grains, lean proteins, and vegetables.
Ask a nutritionist for a meal plan that fits your needs.
Learn about portion sizes and meal timing.
Physical activity helps control blood sugar and improves blood flow to gums.
Aim for 30 minutes of exercise most days.
Walking, swimming, and cycling are good options.
Quit smoking to improve oral health.
Smoking slows healing and increases infection risk.
Ask your doctor about quit-smoking programs.
Healthy choices include:
- Drinking plenty of water
- Eating regular meals
- Avoiding tobacco products
- Getting enough sleep
Community health workers can offer support and education.
Look for local programs that help with diabetes and healthy living skills.
Dental Care and Professional Support
People with diabetes need extra dental care and support from their dentist and healthcare team.
Together, these professionals can prevent and treat oral health problems linked to diabetes.
Importance of Regular Dental Visits
Visit your dentist every six months for dental checkups.
People with diabetes may need to visit more often.
Dentists can spot problems early.
They check for gum disease, infections, and other issues.
Early treatment works better than waiting.
What happens during dental visits:
- Teeth cleaning and exam
- Gum health check
- X-rays when needed
- Blood sugar discussion
Tell your dentist about your diabetes.
Share information about your blood sugar levels and medications.
This helps them give you better care.
Your dentist may suggest check-ups every three to four months.
This depends on your diabetes control and gum health.
Treatments and Interventions for Oral Complications
When we have oral health problems, several treatments can help. The type of treatment depends on how serious the problem is.
Common dental treatments for diabetes patients:
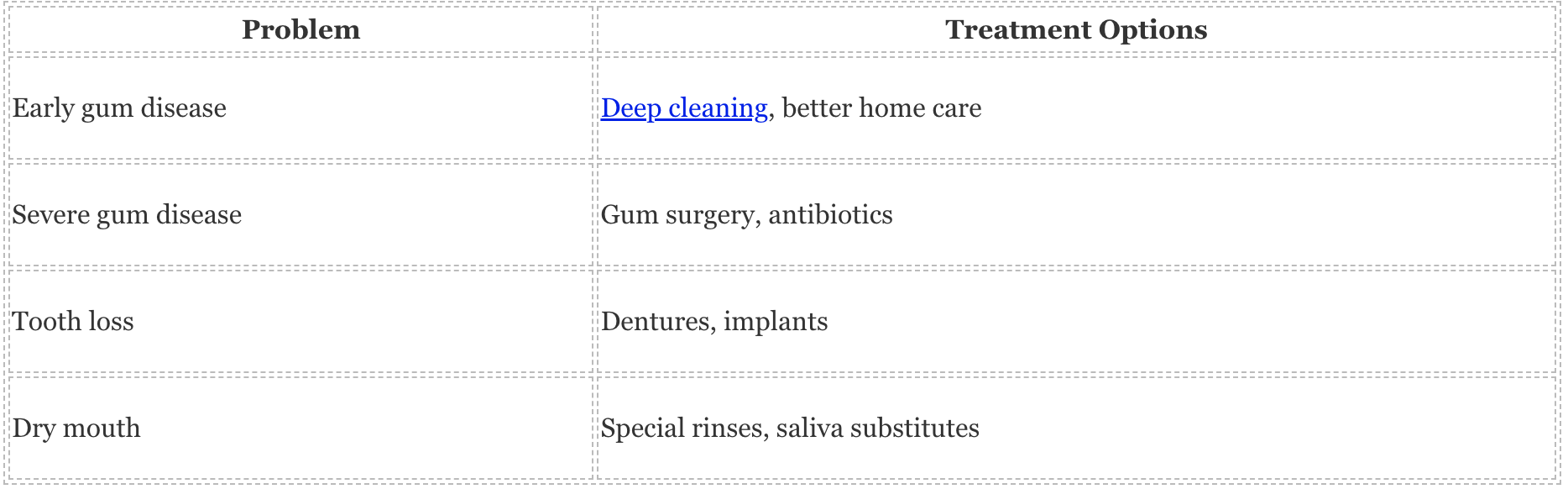
Dentists remove bacteria below the gum line through deep cleaning. This treatment often takes several visits.
Sometimes, dentists prescribe antibiotics to help fight infection. A periodontist treats serious gum disease and performs gum surgery when needed.
This specialist has extra training in gum problems. People who lose teeth may need dentures.
Good blood sugar control helps dentures fit better and heal faster.
Collaboration With the Diabetes Care Team
Our diabetes care team works with our dentist. This team includes our doctor, diabetes educator, and other specialists.
We should tell our doctor about dental problems. Some infections make blood sugar harder to control.
Our doctor may change diabetes medications before dental treatment.
Important information to share:
- Current blood sugar levels
- Diabetes medications we take
- Any dental infections or pain
- Planned dental procedures
Dentists may talk to our doctor before big procedures. They want to make sure we are healthy enough for treatment.
Frequently Asked Questions
Diabetes affects oral health in many ways. High blood sugar levels help bacteria grow and slow healing in the mouth.
How does type 2 diabetes contribute to dental problems?
Type 2 diabetes raises blood sugar levels throughout the body. High glucose in saliva feeds harmful bacteria in the mouth.
These bacteria produce acids that attack tooth enamel. The acids cause cavities and tooth decay to develop faster.
Diabetes also reduces blood flow to the gums. Poor circulation makes it harder for gum tissue to stay healthy and fight infection.
What is the most prevalent oral complication associated with diabetes?
Gum disease is the most common oral problem for people with diabetes. About 95% of adults with diabetes develop some form of gum disease.
The condition starts as gingivitis with red, swollen gums that bleed easily. Without treatment, it progresses to periodontitis.
Periodontitis destroys the tissues and bone that support teeth. This advanced gum disease can lead to tooth loss.
What treatment options are available for gum disease in diabetic patients?
Dentists remove plaque and tartar buildup below the gum line with professional cleanings. Diabetic patients should have cleanings every three to four months.
Scaling and root planing smooth rough spots on tooth roots where bacteria collect. Antibiotic treatments help control bacterial infections in severe cases.
Some patients need surgery to repair damaged gum tissue.
Are people with diabetes more susceptible to tooth loss?
People with diabetes lose teeth at twice the rate of those without diabetes. Poor blood sugar control increases this risk.
Gum disease is the main cause of tooth loss in diabetic patients. The infection destroys the bone and tissue that hold teeth in place.
Diabetic patients also heal more slowly after dental procedures. This makes it harder to save damaged teeth with treatment.
Can diabetes lead to specific symptoms in the mouth?
Dry mouth is a common symptom for diabetic patients. High blood sugar reduces saliva production.
Many patients feel a burning sensation on their tongue or in their mouth. This symptom often gets worse when blood sugar levels are high.
Bad breath that smells fruity or sweet can signal poor diabetes control. Some patients also notice a metallic taste in their mouth.
What oral manifestations are commonly found in persons with diabetes?
White patches called thrush can appear on the tongue and inside the cheeks. High blood sugar helps this fungal infection grow.
Sores or cuts in the mouth may heal slowly. Even small injuries can take weeks to get better.
Swollen and bleeding gums may pull away from the teeth. Tooth mobility and gaps between teeth may also occur.
📞 Contact Kaufman Dentistry Today
Give us a call at (310) 838-7780 to schedule your appointment and take the first step towards a stunning smile.
You can find us at 10760 Washington Blvd., Culver City, CA 90232. We look forward to welcoming you to our practice and helping you achieve the smile of your dreams!
